A 51 year old male patient came to the OPD with chief complaints of shortness of breath since 2 months
Hi, I am greeshmaA, 6th Sem Medical Student.This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
51M farmer by occupation , resident of nalgonda ,came to opd with c/o shortness of breath since 2 months
HOPI
Patient was apparently asymptomatic 2 months ago then he developed SOB of insidious onset, gradually progressive increasing in intensity since 2 months (Glade II- III)
No h/o constipation , nausea , vomiting ,burning micturation
PAST HISTORY :
N/k/c/o DM , HTN , CAD,TB, epilepsy , thyroid disorders
FAMILY HISTORY :
not significant
PERSONAL HISTORY :
Decreased apetite
Mixed diet
Decreased bowel movements
Normal micturation
No known allergies
Alcoholic since 3 yrs
GENERAL EXAMINATION :
I have examined the patient after taking prior consent and informing the patient in the presence of a attendant. The examination was done in both supine and sitting position in a well lit room.
- patient was conscious, coherent and cooperative
- well oriented to time, place and person
- well built and adequately nourished
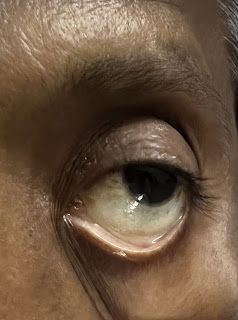
- pallor present
- no icterus
- no cyanosis
- no clubbing of fingers
- no lymphadenopathy
- pitting type pedal
VITALS :
Temperature : afebrile
BP : 100/70 mmhg
Pulse rate : 100/min
Respiratory rate : 16/min
SPO2 : 98% RA
SYSTEMIC EXAMINATION :
CVS :
S1S2 +
Cardiac murmurs heard
No thrills
RS :
Position of Trachea - central
BAE +
NVBS +
P/A :
Soft , Non tender
CNS :
NFND
PROVISIONAL DIAGNOSIS: anemia secondary to blood loss





Comments
Post a Comment